Cognitive Behavioral Therapy, often called CBT, is a structured method that helps individuals recognize how their thoughts set the stage for emotions and behavior. By learning to detect and replace unhelpful thought patterns, people can respond to life’s challenges with more clarity and balance. While CBT is frequently used to treat anxiety, depression, phobias, and panic disorders, it also supports personal growth and everyday emotional resilience.
From Theory to Practice: How CBT Was Born
In the 1960s, psychiatrist Aaron Beck began noticing something profound while treating patients with depression: their emotional suffering often stemmed not from events themselves but from the way they interpreted those events. These distorted interpretations — later termed cognitive distortions — became the foundation of cognitive therapy. When Beck’s approach later integrated the principles of behavioral psychology, Cognitive Behavioral Therapy emerged as a method both practical and deeply evidence-based.
Today, CBT stands as one of the most scientifically validated therapies. Research compiled by PubMed and the American Psychological Association (APA) highlights its consistent effectiveness in treating depression, anxiety, obsessive-compulsive disorder, and post-traumatic stress disorder.
The Core Philosophy Behind CBT
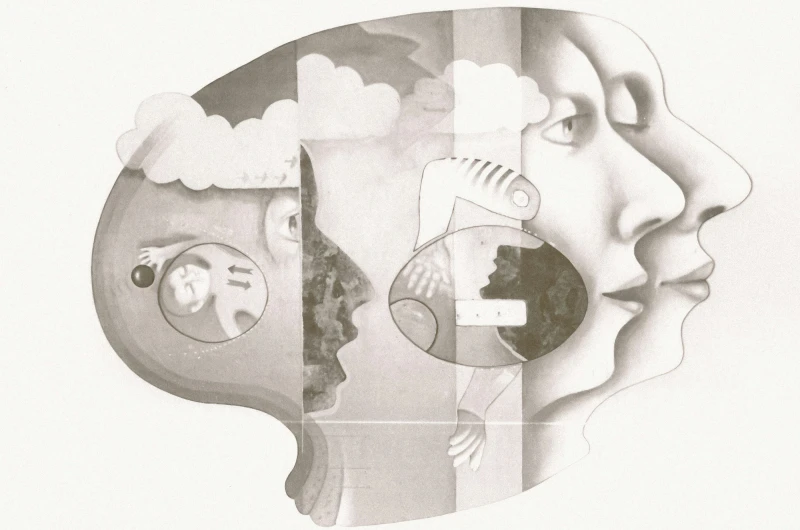
CBT rests on a central truth: emotions are shaped not by what happens to us, but by how we think about what happens. Our thoughts, feelings, and behaviors form a continuous feedback loop. When we adjust one element — say, how we interpret a setback — we inevitably change how we feel and act.
| Component | Meaning | Example |
|---|---|---|
| Thought | How you interpret a situation | “If I make a mistake, I’ll disappoint everyone.” |
| Emotion | The feeling born from that interpretation | Anxiety, guilt, shame |
| Behavior | Action that follows the emotion | Avoiding new challenges |
CBT encourages people to slow down their mental “autopilot,” examine these thought-emotion-behavior links, and replace exaggerated or self-critical thinking with more balanced perspectives. It’s less about forced positivity and more about developing an accurate, compassionate view of oneself and reality.
CBT in Action: Transformative Techniques
1. Cognitive Restructuring
This core exercise helps detect irrational or perfectionistic thoughts and reframe them into constructive alternatives. For example, turning “I must never fail” into “Learning involves trial and error — and that’s progress.”
2. Behavioral Experiments
CBT often uses real-world “experiments” to test negative assumptions. If someone fears judgment, they might deliberately speak up during a meeting and later reflect on how others actually responded — often discovering that the imagined criticism never happened.
3. Gradual Exposure
Used to address phobias and chronic anxiety, this technique helps people face their fears step by step. By repeatedly encountering discomfort in safe, structured ways, the brain learns that fear can fade instead of control us.
4. Thought and Emotion Journaling
Tracking thoughts, emotions, and situations helps reveal hidden patterns. Over time, people start to recognize triggers and break recurring mental habits, cultivating emotional awareness and self-regulation.
What CBT Helps With
According to the World Health Organization (WHO) and the Mayo Clinic, CBT has demonstrated success in addressing:
- Depression and chronic low mood;
- Generalized anxiety and panic disorders;
- Social anxiety and specific phobias;
- Obsessive-compulsive disorder (OCD);
- Post-traumatic stress disorder (PTSD);
- Sleep problems and chronic pain syndromes;
- Disordered eating patterns.
CBT may be applied alone or combined with medication, depending on individual needs — decisions that should always be made in consultation with a qualified clinician.
Scientific Evidence and Long-Term Impact
Research summarized by Harvard Health Publishing shows that CBT’s results often parallel those of antidepressant medications for mild to moderate depression. More importantly, CBT equips people with lifelong tools — preventing relapse by teaching how to manage difficult emotions and future setbacks with self-awareness.
Inside a CBT Program
Most CBT programs consist of 10 to 20 weekly sessions. Early meetings focus on defining specific goals. As therapy progresses, clients learn to observe their thought patterns, apply practical techniques, and reflect on their outcomes. Homework assignments bridge the gap between sessions and daily life, ensuring progress translates into action.
Answer: Self-help books and digital CBT programs exist, but when symptoms are intense or persistent, professional support significantly improves results.
Question: Is CBT suitable for everyone?
Answer: While no therapy fits all, CBT remains one of the most versatile, empirically backed approaches in modern psychology.
Question: When can improvement be expected?
Answer: Some clients report relief after a few sessions, but stable transformation emerges through consistent practice and engagement.
How to Find a Skilled Therapist
Choose a licensed CBT therapist with proven experience. The best practitioners don’t just listen — they actively collaborate, helping clients spot thinking traps, set behavioral goals, and celebrate small wins along the way.
- What beliefs have shaped your reactions lately?
- What could shift if you challenged one recurring negative thought today?
Conclusion
Cognitive Behavioral Therapy offers more than symptom relief — it’s a roadmap for mental clarity and resilience. It empowers individuals to understand their own minds, confront distorted thinking, and rewrite internal narratives. In a world overflowing with stress and uncertainty, mastering your thoughts may be the most profound form of self-care.
Disclaimer: This content is for informational and educational purposes only and should not replace a consultation with a psychologist, psychiatrist, or licensed mental health provider. If you’re experiencing symptoms of depression, anxiety, or emotional distress, seek professional guidance.


